Sick people as passive recipients of the superior medical knowledge? Medicine as a purely functional means of treatment? Such ideas are obsolete – the focus of the healthcare industry and market research is on patients. Patient Centricity is certainly disruptive in nature. This is reflected in digitalization and easy access to medical information, doctor reviews, drug prices and alternative therapies: consumption of medicine and healthcare are in the foreground, patients have the choice, and pharmaceutical companies realize that a differentiated understanding of life, experiences, the most important needs and challenges of their patients is required.
Active role of pharmaceutical research
At Borderless Access, we wanted to better understand this trend, identify risks and challenges, and outline the opportunities for healthcare market research to take an active role in patient centricity. In a case study using the example of an emerging country (Indonesia) and a developed country (UK), we found out how digital technologies help to promote patient centricity and improve health outcomes. With our healthcare panels, which provide global access to almost 700,000 healthcare players, 1,600 patients and 100 general practitioners in Indonesia and the UK were initially surveyed about clarity and comprehensibility in doctor-patient communication.
Communication? Optimizable!
In both countries, a decoupling in terms of the doctor-patient relationship and communication was observed: In the UK, 56 percent of patients said they felt unsure about what the doctor might have actually meant and were of the opinion that the doctor would articulate too briefly. Doctors, in turn, criticized a lack of adherence to therapy and high patient demands (43 percent). In Indonesia, 53 percent of patients were of the opinion that the doctor communicated inadequately and there was uncertainty about what was actually communicated. 58 percent of Indonesian doctors complained about high patient demands and a lack of adherence to therapy.
Uncover the inarticulate – with smart devices
The question arose: How can healthcare market research close the gap between inarticulate, subjective and non-communicative information for the benefit of patients? In a follow-up study, the patient journey was mapped and recorded and monitored using a smart device from initial awareness of the problem to treatment. Information was collected on gender, age 25 and over, lifestyle diseases, ownership of a smart device (wearables), social status, general standard of living and access to high-quality healthcare, sanitary facilities and housing. Data such as blood volume pressure, heart rate, skin temperature and muscle tone, GPS data and general activity level were monitored in parallel via the smart device.
Patient Centricity Scenarios
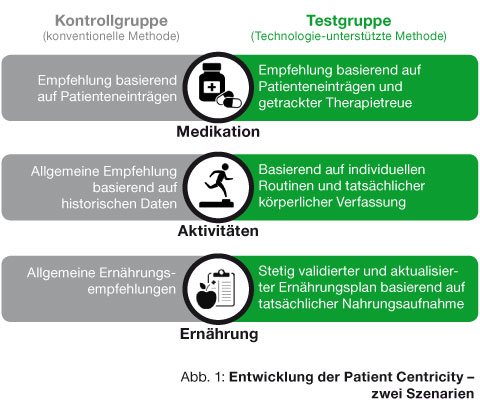
When comparing the test group (technology-supported method) and the control group (conventional method, Fig. 1), the following possible scenarios of how patient centricity can develop were defined:
Scenario 1: Patient Submits Minimal Details
Doctors must realize the need to examine the patients through passive data monitoring to get a personalized and effective diagnosis that includes accurate laboratory tests, medication and follow-up visits and so on. The result: conventional advice in which the doctor only prescribes medication.
Scenario 2: Patient submits additional information
Doctors can validate this for precision diagnostics – from passive data monitoring to medication to follow-up examinations. The doctors not only prescribe medication, the level of advice exceeds that of scenario 1 and also addresses factors such as diet and exercise that shorten treatment time. In the control group, medication was based on information from the patient, whereas in the test group, tracked treatment adherence was also taken into account. The activity recommendation was based on historical data (control group) and was generic in nature, whereas in the test group the recommendation was based on individual routines and actual physical condition (test group). As far as the information about the nutritional routine in the control group was concerned, only general recommendations were made, whereas in the test group if food intake was missed, this was validated and included in the nutritional plan in an updated form.
Satisfied patients, satisfied doctors
The results of the follow-up study showed that the test group was able to minimize the communication gap between doctor and patient in both the UK and Indonesia. In the UK only 44 percent of patients said they felt inadequately informed (versus 56 percent in advance), in Indonesia it was 37 percent (versus 53 percent). Only 39 percent (versus 43 percent) of doctors also criticized differing treatment adherence and patient demands; in Indonesia only 51 percent (versus 58 percent) criticized this.
How tracking can refine feedback
The pioneering approach to patient centricity represents a combination of both methods. In emerging markets, innovation is driven by technology and human capital. In developed countries, patients rely on health apps, patient groups and real-time feedback tools.
In healthcare market research, a rethink is necessary away from conventional feedback methodology. Existing quality and quantity of patient information that can be captured via smart devices will methodically change feedback. It has never been easier to map a patient’s lifestyle and the patient journey; tracking studies as a hybrid of technical and traditional surveys are becoming the new standard. The data collected using passive technologies must be validated and analyzed in new depth by market research companies.
About the author:
As Vice President Europe , Max Czycholl leads all business and sales activities of Borderless Access in Europe from the new Hamburg office. He has twelve years of market research experience, was most recently Director Healthcare at Dynata (formerly Research Now) and has been a thought leader in healthcare market research for many years.







